“Altered T cells in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)”
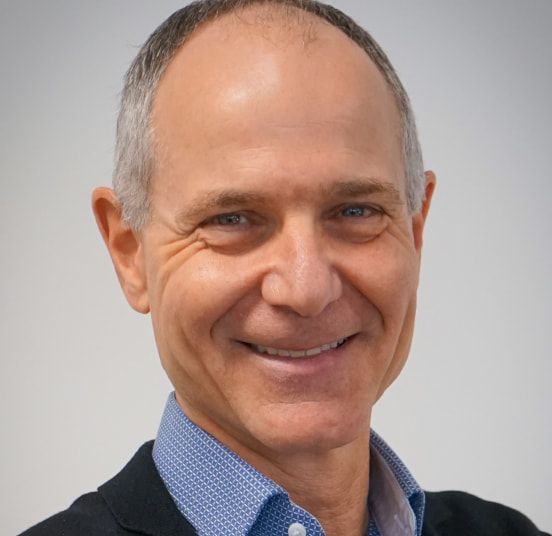
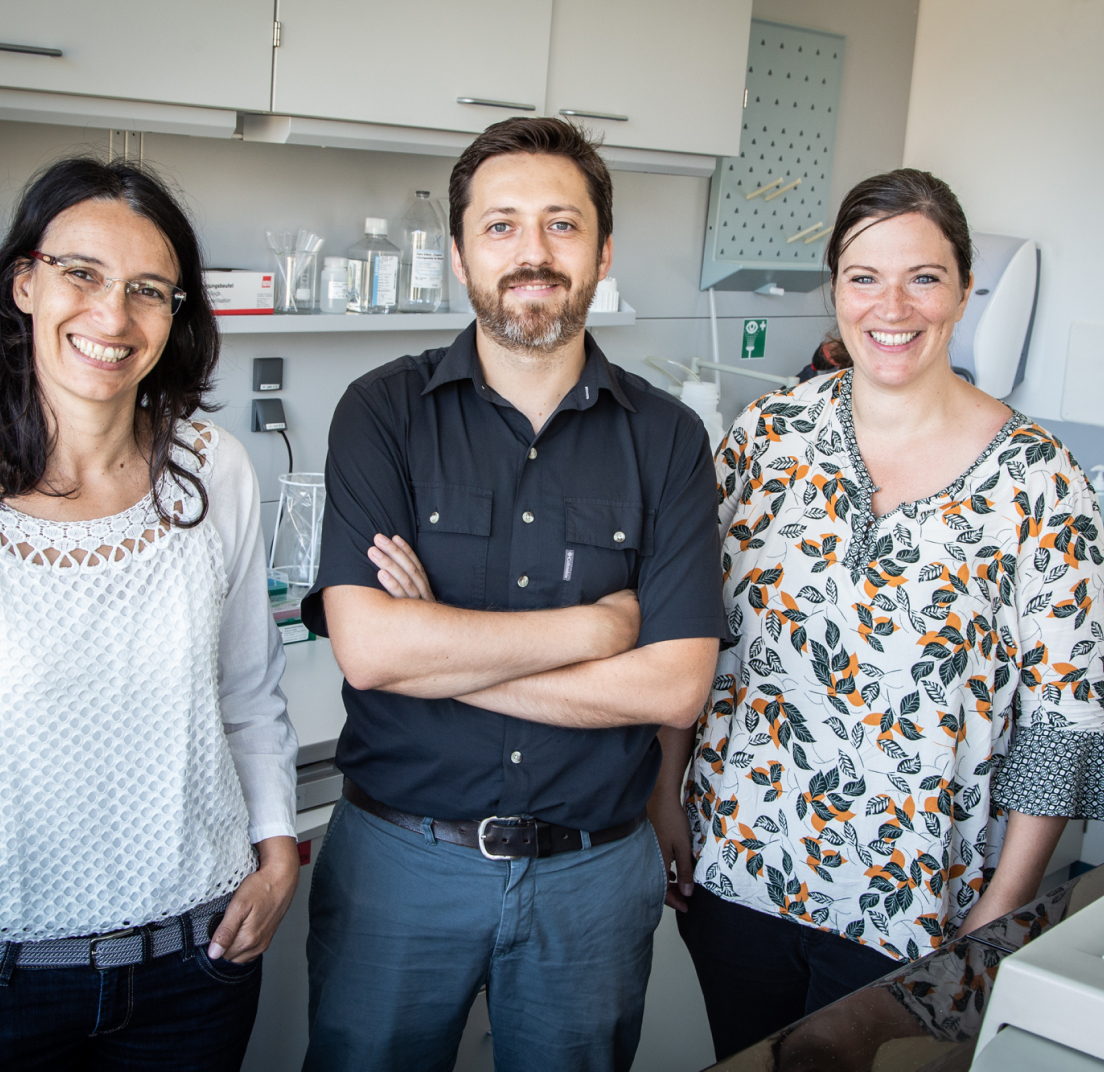
Principal Investigators: Liisa Selin (PhD), Anna Gil (PhD)
University of Massachusetts Medical School
- Home
- >
- Liisa Selin and Anna Gil
Liisa Selin and Anna Gil
“Altered T cells in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)”
Principal Investigators: Liisa Selin (PhD), Anna Gil (PhD)
University of Massachusetts Medical School

Liisa Selin, PhD, is a University of Massachusetts Medical School researcher with deep knowledge of immune defense against viruses. Dr. Selin and her co-PI, Anna Gil, PhD, will examine the role of specific immune cells – called T cells – that play a key role in tailoring the body’s immune response. The researchers previously identified elevated numbers of a subset of T cells in blood samples from people with ME/CFS. This study is designed to uncover whether these cells reflect a specific infectious or autoimmune response that could be driving immune dysfunction in ME/CFS.
Major Ramsay goal fulfilled:
✓ Received a $2.5 million R01 grant from the National Institutes of Health (NIH) to study the role of aberrant T cell responses in the immunopathogenesis of ME/CFS patients.
“We are personally aware of the devastation that ME/CFS causes and the challenge of surviving each day with this disease. We are therefore very excited by our recent findings of a unique subset of T cells that may play a role in ME/CFS immunopathogenesis and its potential to be a biomarker. We greatly appreciate the support of the Ramsays in supporting us to continue our research into ME/CFS.”
– Liisa Selin and Anna Gil
Read the research study abstract below:
Our understanding of the immunological defects present in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is severely lacking compared to other disorders, leading to a major barrier to research, diagnosis, and treatment. ME/CFS is a complex disorder affecting numerous organ systems and biological processes with studies focusing on changes in cytokines, metabolism, and identifying a potential causative infectious agent. In this pilot study, we propose to examine the role of a novel subset of immune cells, CD4+CD8+ T cells in the pathology of ME/CFS.
We recently discovered not only an increased frequency of this otherwise rare T cell in a group of ME/CFS patients we were studying, but also that they were highly activated producing unusual cytokines. We observed a difference in the activation profile of these cells in mild and severe cases of ME/CFS. In my long career of studying human T cell responses during viral infections I have never previously observed an increase in this cell type. We will examine the role they may play in the highly dysregulated immune response of ME/CFS patients. Much of the published data seems to suggest that ME/CFS may be preceded by infection, and the chronic manifestation of illness may represent an altered host response to infection, or an inability to resolve inflammation.
Based on our preliminary data, we will examine in a larger cohort, whether this unique subset of CD4+CD8+ T cells is increased in all ME/CFS donors, or does it only occur in a subgroup. We will also assess its role in mediating the disease by examining its frequency and alterations in its function in ME/CFS patients, manifesting either a mild or severe form of the disease as compared to healthy donors. Also, T cells have unique receptors (TCR) that they use to recognize foreign pathogens and eliminate them. Sometimes these TCR also inadvertently recognize self-proteins and lead to autoimmune diseases.
In our preliminary studies examining the TCR repertoire of the CD4+CD8+ population there was strong evidence they were expanded by recognizing an antigen. At this time, we do not know if this is a self or a pathogen antigen. We will therefore explore the TCR repertoire of this unique population of CD4+CD8+ T cells in order to find characteristics that will help us identify the potential antigen that is driving their expansion and activation. This would be a major step in the field potentially leading to the identification a specific infectious or autoimmune response that could be the main driver of the immunological basis of ME/CFS. Studying these unique cells (CD4+CD8+ T cells) in a larger population of ME/CFS patients has the potential to give us a biomarker (much needed for this disease) while giving us clues to the mechanisms driving the pathology of ME/CFS and thus therapy.
Learn more about the Ramsay Grants
Meet the Researchers
Learn more
Apply for a Grant
Learn more