Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a chronic, complex, neuroimmune disease that profoundly limits the health and productivity of patients and, like Long Covid, is often triggered by an infection.
At this time, the cause of ME/CFS is not fully understood. There is no diagnostic test, cure, nor FDA-approved treatments or drugs for ME/CFS, and patients often suffer for life.
While “ME/CFS” is the preferred name by many, this disease has also formerly been known as systemic exertion intolerance disease (SEID), chronic fatigue immunity deficiency syndrome (CFIDS), or post-viral fatigue syndrome (PVFS).
Solve M.E. is a proud co-founder of the World ME Alliance, which produced an ME/CFS Fact Sheet available in multiple language.
Everyone is at risk. ME/CFS may begin as early as age 10 and as late as age 77. It is estimated that between 5 – 9 million Americans suffer from ME/CFS and estimates vary from 17 – 24 million people with ME/CFS worldwide. Although research has shown that ME/CFS is about two to four times more likely to occur in women than men, ME/CFS strikes people from every age, racial, ethnic, and socioeconomic group.
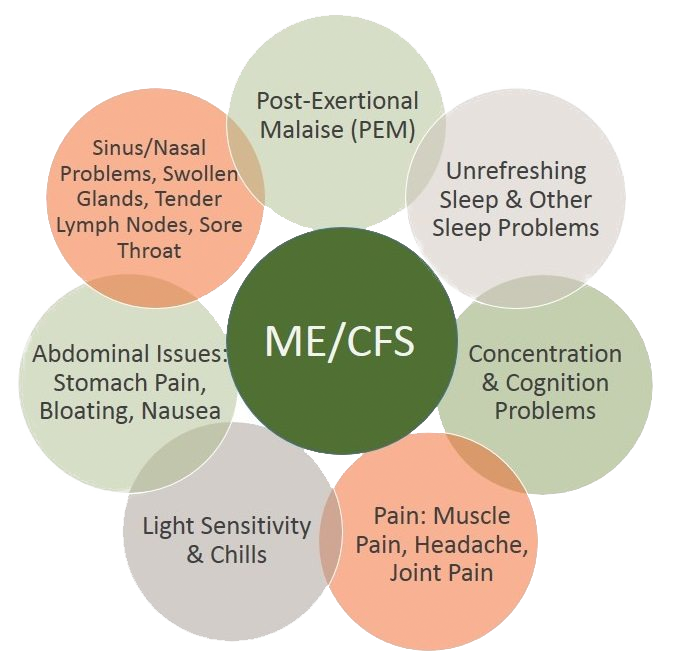
ME/CFS symptoms, which can often be made worse by standing upright, include:
If you think you may have ME/CFS, take our quick online quiz.
Because these symptoms are shared with many other illnesses — and because many of these conditions lack a diagnostic test or biomarker — identifying which illnesses are present can be difficult. Some patients receive diagnoses for multiple conditions. Common conditions that occur along with ME/CFS (co-morbidities) include the following:
There is currently no FDA-approved treatment or drug for ME/CFS. As neither a cause nor cure for ME/CFS has been identified, treatment is directed at relieving symptoms. However, there are interventions and symptom-reduction strategies that you can use to significantly improve patients’ quality of life.
Learn more in our “Patient Resources” section.
Studies show that less than 9-16 percent of ME/CFS patients in the United States have been properly diagnosed. Diagnosing ME/CFS is a challenging process because there is still not one diagnostic test or biomarker that’s conclusive. Getting a definitive diagnosis often takes months or even years.
Providing compassionate and effective care for patients with ME/CFS can be challenging, like many other multisystemic chronic conditions. Patients and their providers must be partners with open lines of communication in order to effectively manage this illness. For medical providers seeking to provide better care for ME/CFS patients, reference our educational materials at our Medical Provider Resources page.
The severity of ME/CFS varies greatly from patient to patient, with some people able to maintain fairly active lives. For others, ME/CFS has a profound impact. About 25 percent of people with ME/CFS are housebound or bedbound as a result of their illness. For many, there is often a pattern of relapse and remission. Most symptoms are invisible to others, which makes it difficult for family members, friends, and the public to understand the challenges of the disease.
We know it’s so important to share personal experiences to increase understanding of ME/CFS. Visit our Humans of Chronic Illness story archive to read and share your stories of ME/CFS.
Solve M.E. is also producing Long Haul Voices, a mini-series that amplifies the experiences of individuals with Long Covid and ME/CFS, the experts devoted to improving their care, and the challenges surrounding these largely invisible, poorly-understood diseases that affect a rapidly growing population.

“It feels like I always have the flu, only much worse. It feels like the world is always moving, and I can’t find my bearings.”
Rob P.

“When my symptoms first occurred, I was diagnosed with the flu during June, July, and August during off-flu season. Doctors suspected that I was a hypochondriac.”
Conella B.

“Sometimes it feels as if my body is shutting down on me. Every time I ever have gone to the emergency room for my invisible illnesses, they have never once been able to help me in any way.”
Kelly S.
The cause of ME/CFS may vary from person to person. Some people became sick with ME/CFS following a sudden and severe flu-like illness. Others became sick with ME/CFS gradually over a period of months or years without noticing a specific cause. Research has shown that there is genetic, central nervous system, immune and metabolic factors involved in ME/CFS and scientists are studying these connections to develop diagnostic tests and treatments. Solve M.E. is actively supporting research on diagnosis and treatment.
The time to recovery from ME/CFS varies. Some patients recover in small to moderate degrees, while others recover almost fully, but no one knows why. Others have progressively worse symptoms over time. Unfortunately, very little data exists about recovery rates for ME/CFS. Determining what helps people recover from ME/CFS is an important area of research that Solve
M.E. is actively supporting.
There is currently no diagnostic test for ME/CFS. This is an important area of research that Solve M.E. is actively supporting.
There is currently no cure for ME/CFS but there is evidence that the sooner you get a diagnosis, the greater the chances of recovering. Getting diagnosed early is important!
No, researchers agree that ME/CFS is not a form of depression or psychiatric illness. All chronic illnesses have significant medical, psychological and social components. However, the physical symptoms of ME/CFS differ greatly than those of depression and can help to differentiate between the two. While ME/CFS is not a psychological disorder, depression or anxiety may occur as a result of having any chronic, debilitating illness.
Founded in 1987, Solve M.E. the longest standing organization serving ME/CFS patients and advancing rigorous research. Despite the fundamental complexity of this illness, we believe that ME/CFS can and will be solved in our lifetime.
350 N Glendale Ave.
Suite B #368
Glendale, CA 91206
SolveCFS@SolveCFS.org
704-364-0016
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |
Please let us know more about you.
Please let us know more about you.
Please let us know more about you.